We usually think of food as energy and raw materials, but food can also “talk” to our genes. This secret conversation between nutrients and genes influences how our brains and bodies function, down to the cellular and molecular levels.
We want to decipher the different types of food messages and decode how they affect brain, behavior, and the risk for disease.
DIET, GENES, & TASTE
Can we train our taste buds for health?

Monica Dus, University of Michigan
Have you ever wondered why only hummingbirds sip nectar from feeders?
Unlike sparrows, finches and most other birds, hummingbirds can taste sweetness because they carry the genetic instructions necessary to detect sugar molecules.
Like hummingbirds, we humans can sense sugar because our DNA contains gene sequences coding for the molecular detectors that allow us to detect sweetness.
But it is more complex than that. Our ability to sense sweetness, as well as other tastes, involves a delicate dance between our genetic makeup and the foods we encounter from the womb to the dinner table.
Neuroscientists like me are working to decipher how this intricate interplay between genes and diet shapes taste.
In my laboratory at the University of Michigan, we are diving deeply into one specific aspect, which is how consuming too much sugar dulls the sense of sweetness. Taste is so central to our eating habits that understanding how genes and the environment shape it has crucial implications for nutrition, food science and disease prevention.
The role of genes in sensing taste
As with hummingbirds, the human ability to discern what food tastes like depends on the presence of taste receptors. These molecular detectors are found on the sensory cells, which are housed inside the taste buds, the sensory organs on the surface of the tongue.
The interactions between taste receptors and food molecules give rise to the five basic taste qualities: sweetness, savoriness, bitterness, saltiness and sourness, which are transmitted from the mouth to the brain via specific nerves.
For instance, when sugar binds to the sweet receptor, it signals sweetness. Our innate preference for the taste of some foods over others is rooted in how the tongue and the brain became wired during our evolutionary history. Taste qualities signaling the presence of essential nutrients and energy, like salt and sugar, send information to brain areas linked to pleasure. Conversely, tastes that alert us to potentially harmful substances, such as the bitterness of certain toxins, are connected to those that make us feel discomfort or pain.
While the presence of genes encoding for functional taste receptors in our DNA allows us to detect food molecules, how we respond to these also depends on the unique combination of taste genes we carry. Like ice cream, genes, including those for taste receptors, come in different flavors.
Take, for instance, a taste receptor for bitterness called TAS2R38. Scientists found small changes in the genetic code for the TAS2R38 gene among different people. These genetic variants affect how people perceive the bitterness of vegetables, berries and wine.
Follow-up studies have suggested a link between those same variants and food choice, particularly with respect to vegetable and alcohol consumption.
Many more variants exist in our gene repertoire, including those for the sweet taste receptor. However, whether and how these genetic differences affect our taste and eating habits is still being worked out. What is certain is that while genetics lays the groundwork for taste sensations and preferences, experiences with food can profoundly reshape them.
How diet influences taste
Many of our innate sensations and preferences are molded by our early experiences with food, sometimes before we’re even born. Some molecules from the mother’s diet, like garlic or carrots, reach the fetus’s developing taste buds via the amniotic fluid and can affect the appreciation of these foods after birth.
Infant formula can also influence food preferences later on. For example, research shows that infants fed with formulas that are not based on cow’s milk – which are more bitter and sour because of their amino acid content – are more accepting of bitter, sour and savory foods such as vegetables after weaning than those who consume cow milk-based formula. And toddlers who drink sweetened water strongly prefer sweet beverages as early as age 2.
The effect of food on our taste predispositions doesn’t stop in early life: What we eat as adults, especially our sugar and salt intake, can also shape how we perceive and potentially choose food. Cutting down on sodium in our diet decreases our preferred level of saltiness, whereas consuming more makes us like saltier foods.
Something similar occurs with sugar: Reduce sugar in your diet and you may find food sweeter. Conversely, as research in rats and flies suggests, high sugar levels may dull your sensation of sweetness.
Although we researchers are still working out the exact how and why, studies show that high sugar and fat intake in animal models dampens the responsiveness of taste cells and nerves to sugars, modifies the number of taste cells available and even flips genetic switches in the taste cells’ DNA.
In my lab, we’ve shown that these taste alterations in rats return to normal within weeks when the extra sugar is removed from the diet.

Illness can also influence taste
Genetics and food aren’t the only factors that affect taste.
As many of us discovered during the height of the COVID-19 pandemic, disease can also play a role. After testing positive for COVID-19, I couldn’t tell the difference between sweet, bitter and sour foods for months.
Researchers have found that about 40% of people infected with SARS-CoV-2 experience impairment in taste and smell. In about 5% of those people, these taste deficits persist for months and years.
Although researchers don’t understand what causes these sensory alterations, the leading hypothesis is that the virus infects the cells that support the taste and smell receptors.
Training taste buds for healthier eating
By shaping our eating habits, the intricate dance between genes, diet, disease and taste can affect the risk for chronic diseases.
Beyond distinguishing food from toxins, the brain uses taste signals as a proxy to estimate the filling power of foods. In nature, the stronger a food tastes – in terms of sweetness or saltiness – is directly connected to its nutrient levels and calorie content. For example, a mango contains five times the amount of sugar than a cup of strawberries, and this is why it tastes sweeter and is more filling. Thus, taste is important not just for food enjoyment and choice, but also for regulating food intake.
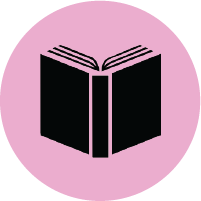
When taste is altered by diet or disease, sensory and nutrient information could become “decoupled” and no longer provide accurate information to our brains about portion size. Research shows this may also occur with consumption of artificial sweeteners.
And indeed, in recent studies in invertebrate animal models, our lab discovered that the changes in taste caused by high dietary sugar intake drove higher eating by impairing these food predictions. Notably, many of the eating patterns and brain changes we observed in flies have also been discovered in people who ate foods high in sugar or fat or who had high body-mass index. This raises the question of whether these effects also arise from taste and sensory alterations in our brains.
But there is a silver lining to the adaptable nature of taste. Since diet shapes our senses, we can actually train our taste buds – and our brains – to respond and prefer foods with lower quantities of sugar and salt.
Interestingly, many people already say that they find foods overly sweet, which may not be surprising since between 60% to 70% of grocery store foods contain added sugar. Reformulating foods tailored to our genes and the plasticity of our taste buds could be a practical and powerful tool to enhance nutrition, promote health and decrease the burden of chronic disease.
Monica Dus, Associate Professor of Molecular, Cellular, and Developmental Biology, University of Michigan
This article is republished from The Conversation under a Creative Commons license. Read the original article.
HOW HIGH DIETARY SUGAR DULLS SWEETNESS
Above we explained how taste sensation is shaped by diet. In the lab, we examined the effects of high dietary sugar on taste sensation. Our experiments in flies and rats show that eating elevated sugar levels leads to the desensitization of the taste cells and nerves to sweetness. This decrease in responses of the taste system to some sweet stimuli leads to animals sensing food as less sweet than before, which has significant consequences for food intake through changes in dopamine transmission (see below).

High sugar levels dull taste by enhancing the silencing activity of a nutriepigenetic pathway composed of the conserved nutrient-sensor O-GlcNAc Transferase and the epigenetic repressor Polycomb Repressive Complex 2.1. OGT and PRC2.1 interact at the level of chromatin to instruct changes in chromatin accessibility in response to the dietary environment, which results in the silencing of several hundreds of genes involved in synaptic function, morphology, and plasticity. Recent work shows that neural activity plays an important role in this nutrigenomic silencing by proving the taste cells with the neural activity information.
We propose that nutrigenomic mechanisms can be thought as a new path of information flow in biological systems. Their function is to amplify transient, and often small, variations in nutrient and activity levels, into robust reactions that can orchestrate responses to current and future environmental challenges.
HOW HIGH DIETARY SUGAR STIMULATES EATING
Consumption of diets high in refined sugar and saturated fat is associated with higher food intake in humans and animal models. Over time, this can lead to metabolic and chronic diseases (diabetes, heart, cancer), which decrease life quality and expectancy. To understand how these foods stimulate eating, we investigated the effects of high sugar on the brain pathways important for regulating food intake.
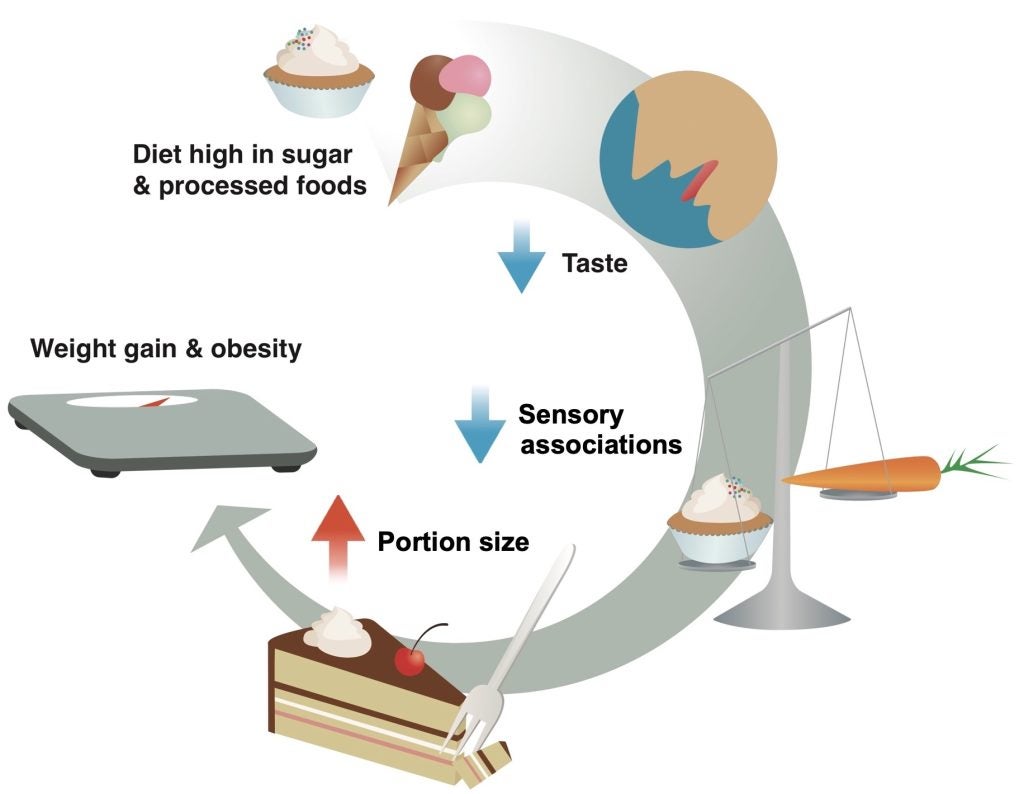
We found that high sugar desensitizes the responses of the taste cells and nerves to sweet stimuli; this was dependent on diet, not obesity. We further demonstrated that this dulling of sweet taste decreased the activity of dopaminergic neurons and of downstream circuits important for satiety, such as those involved in forming food memories. This led animals to consume longer and larger meals, which over time promoted weight gain and metabolic disease. We showed that these changes in taste, dopamine transmission, and food memories were all dependent on dietary metabolite, not obesity. This suggests that sugar perturbs brain processes early to drive metabolic disease. In these published works we also revealed that the alterations in dopamine and memory circuits are the consequence of taste changes (described above). This is because taste signals are important for many aspects of eating; beyond detecting and savoring foods., taste sensations (and flavor more broadly) also affect satiety.
Indeed, studies have shown that, rather than relying on digestive and hormonal signals, animals use the sensory intensity of food to decide how much to eat during meals. Since foods that are sweeter or creamier, also have more calories, these sensations serve as “cues” to estimate the filling power of food and determine portion size.11–13,56 When taste and flavor sensations are modified by the high amounts of salt, sugar, and fat, these predictions may no longer function as effective estimates of how much to eat. The formation of food predictions requires dopamine transmission, which occurs when animals eat something salient, such as ice cream.14,57,58 Lower taste intensity could diminish the responses of dopaminergic neurons and prevent the formation or lower the strength of the predictions. Our results suggest that is the case: fruit flies fed a high sugar diet showed lower dopaminergic transmission 59 and ineffective food predictions, which led to larger meals and obesity; these were entirely dependent on sensory changes. Rodents and humans fed high fat and sugar diets experience similarly profound alterations and disruptions in dopaminergic transmission and reinforcement learning, although the causes remain unknown.18,60–64 For example, people who consume ice cream daily for two weeks have lower responses in the striatum and insula to milkshakes.65 Could some of these disruptions arise from the reshaping of our taste system by dietary exposure to high salt, sugar, and fat?
Besides weakening the efficiency of food predictions, diet-induced sensory alterations could also enhance our desire for food by creating a mismatch in the number of calories expected versus those actually received.66,67 Imagine expecting to eat a carrot, only to be served carrot cake: your dopaminergic system would sizzle. In humans, rodents, and even flies, these types of sensory-nutrient mismatches change the reinforcing properties of food and increase our wanting for it (incentive-sensitization).3,56,68–71 We are currently investigating this question. Finally, since sensory signals also prepare the body to receive food, sensory-nutrient mismatches could also affect its metabolization.72,73 Indeed, in a recent human study, the uncoupling between sensory and nutrient signals in carbohydrate-containing foods impaired glucose metabolism.74
We propose that the reshaping of taste sensation by diets high in salt, sugar, and fat – could drive both a decrease in the satiating power and a higher desire for food. Our results are in line with this hypothesis.
WHAT IS NUTRIGENOMICS?
People typically think of food as calories, energy and sustenance. However, the latest evidence suggests that food also “talks” to our genome, which is the genetic blueprint that directs the way the body functions down to the cellular level.
This communication between food and genes may affect your health, physiology and longevity. The idea that food delivers important messages to an animal’s genome is the focus of a field known as nutrigenomics. This is a discipline still in its infancy, and many questions remain cloaked in mystery. Yet already, we researchers have learned a great deal about how food components affect the genome.
The interaction of food and genes
If the idea that food can drive biological processes by interacting with the genome sounds astonishing, one need look no further than a beehive to find a proven and perfect example of how this happens. Worker bees labor nonstop, are sterile and live only a few weeks. The queen bee, sitting deep inside the hive, has a life span that lasts for years and a fecundity so potent she gives birth to an entire colony.
And yet, worker and queen bees are genetically identical organisms. They become two different life forms because of the food they eat. The queen bee feasts on royal jelly; worker bees feed on nectar and pollen. Both foods provide energy, but royal jelly has an extra feature: its nutrients can unlock the genetic instructions to create the anatomy and physiology of a queen bee.
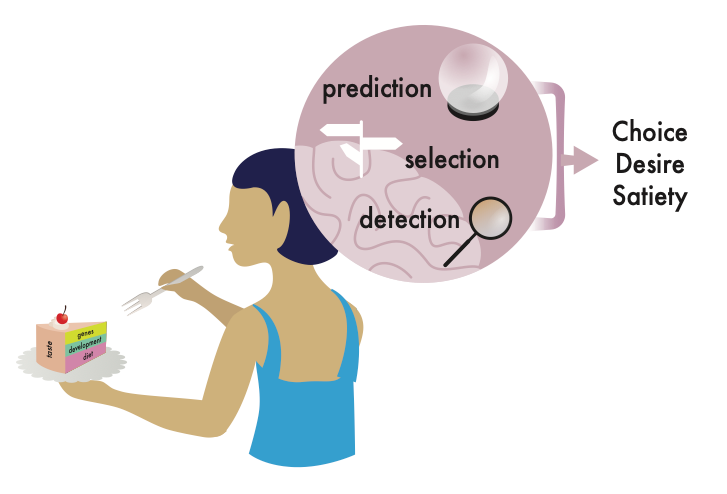
So how is food translated into biological instructions? Remember that food is composed of macronutrients. These include carbohydrates – or sugars – proteins and fat. Food also contains micronutrients such as vitamins and minerals. These compounds and their breakdown products can trigger genetic switches that reside in the genome.
Like the switches that control the intensity of the light in your house, genetic switches determine how much of a certain gene product is produced. Royal jelly, for instance, contains compounds that activate genetic controllers to form the queen’s organs and sustain her reproductive ability. In humans and mice, byproducts of the amino acid methionine, which are abundant in meat and fish, are known to influence genetic dials that are important for cell growth and division. And vitamin C plays a role in keeping us healthy by protecting the genome from oxidative damage; it also promotes the function of cellular pathways that can repair the genome if it does get damaged.
Depending on the type of nutritional information, the genetic controls activated and the cell that receives them, the messages in food can influence wellness, disease risk and even life span. But it’s important to note that to date, most of these studies have been conducted in animal models, like bees.
Interestingly, the ability of nutrients to alter the flow of genetic information can span across generations. Studies show that in humans and animals, the diet of grandparents influences the activity of genetic switches and the disease risk and mortality of grandchildren.
Cause and effect
One interesting aspect of thinking of food as a type of biological information is that it gives new meaning to the idea of a food chain. Indeed, if our bodies are influenced by what we have eaten – down to a molecular level – then what the food we consume “ate” also could affect our genome. For example, compared to milk from grass-fed cows, the milk from grain-fed cattle has different amounts and types of fatty acids and vitamins C and A . So when humans drink these different types of milk, their cells also receive different nutritional messages.
Similarly, a human mother’s diet changes the levels of fatty acids as well as vitamins such as B-6, B-12 and folate that are found in her breast milk. This could alter the type of nutritional messages reaching the baby’s own genetic switches, although whether or not this has an effect on the child’s development is, at the moment, unknown.
And, maybe unbeknownst to us, we too are part of this food chain. The food we eat doesn’t tinker with just the genetic switches in our cells, but also with those of the microorganisms living in our guts, skin and mucosa. One striking example: In mice, the breakdown of short-chain fatty acids by gut bacteria alters the levels of serotonin, a brain chemical messenger that regulates mood, anxiety and depression, among other processes.
Food additives and packaging
Added ingredients in food can also alter the flow of genetic information inside cells. Breads and cereals are enriched with folate to prevent birth defects caused by deficiencies of this nutrient. But some scientists hypothesize that high levels of folate in the absence of other naturally occurring micronutrients such as vitamin B-12 could contribute to the higher incidence of colon cancer in Western countries, possibly by affecting the genetic pathways that control growth.
This could also be true with chemicals found in food packaging. Bisphenol A, or BPA, a compound found in plastic, turns on genetic dials in mammals that are critical to development, growth and fertility. For example, some researchers suspect that, in both humans and animal models, BPA influences the age of sexual differentiation and decreases fertility by making genetic switches more likely to turn on.
All of these examples point to the possibility that the genetic information in food could arise not just from its molecular composition – the amino acids, vitamins and the like – but also from the agricultural, environmental and economic policies of a country, or the lack of them.
Scientists have only recently begun decoding these genetic food messages and their role in health and disease. We researchers still don’t know precisely how nutrients act on genetic switches, what their rules of communication are and how the diets of past generations influence their progeny. Many of these studies have so far been done only in animal models, and much remains to be worked out about what the interactions between food and genes mean for humans.
What is clear though, is that unraveling the mysteries of nutrigenomics is likely to empower both present and future societies and generations.
This article was written by Monica Dus for The Conversation under a Creative Commons license. Read the original article.
HOW DOES FOOD AFFECT THE BRAIN?
During the long seafaring voyages of the 15th and 16th centuries, a period known as the Age of Discovery, sailors reported experiencing visions of sublime foods and verdant fields. The discovery that these were nothing more than hallucinations after months at sea was agonizing. Some sailors wept in longing; others threw themselves overboard. The cure for these harrowing mirages turned out to be not a concoction of complex chemicals, as once suspected, but rather the simple antidote of lemon juice. These sailors suffered from scurvy, a disease caused by a deficiency of vitamin C, an essential micronutrient that people acquire from eating fruits and vegetables.
Vitamin C is important for the production and release of neurotransmitters, the chemical messengers of the brain. In its absence, brain cells do not communicate effectively with one another, which can lead to hallucinations.
As this famous example of early explorers illustrates, there is an intimate connection between food and the brain, one that researchers like me are working to unravel. While we can’t yet prevent or treat brain conditions with diet, researchers like me are learning a great deal about the role that nutrition plays in the everyday brain processes that make us who we are. Perhaps not surprisingly, a delicate balance of nutrients is key for brain health.
Vitamins and mineral deficiencies

As with vitamin C, deficits in other vitamins and minerals can also precipitate nutritional diseases that adversely impact the brain in humans. For example, low dietary levels of vitamin B3/niacin – typically found in meat and fish – cause pellagra, a disease in which people develop dementia.
Niacin is essential to turn food into energy and building blocks, protect the genetic blueprint from environmental damage and control how much of certain gene products are made. In the absence of these critical processes, brain cells, also known as neurons, malfunction and die prematurely, leading to dementia.
In animal models, decreasing or blocking the production of niacin in the brain promotes neuronal damage and cell death. Conversely, enhancing niacin levels has been shown to mitigate the effects of neurodegenerative diseases such as Alzheimer’s, Huntington’s and Parkinson’s. Observational studies in humans suggest that sufficient levels of niacin may protect against these diseases, but the results are still inconclusive. Interestingly, niacin deficiency caused by consumption of excessive amounts of alcohol can lead to similar effects as those found with pellagra.
Ketogenic diet for epilepsy
Not all low levels of something are detrimental to the brain. In fact, studies show that people with drug-resistant epilepsy – a condition in which brain cells fire uncontrollably – can reduce the number of seizures by adopting an ultralow-carbohydrate regimen, known as a ketogenic diet, in which 80% to 90% of calories are obtained from fat.
Carbohydrates are the preferred energy source for the body. When they are not available – either because of fasting or because of a ketogenic diet – cells obtain fuel by breaking down fats into compounds called ketones. Utilization of ketones for energy leads to profound shifts in metabolism and physiology, including the levels of hormones circulating in the body, the amount of neurotransmitters produced by the brain and the types of bacteria living in the gut.
Researchers think that these diet-dependent changes, especially the higher production of brain chemicals that can quiet down neurons and decrease levels of inflammatory molecules, may play a role in the ketogenic diet’s ability to lower the number of seizures. These changes may also explain the benefits of a ketogenic state – either through diet or fasting – on cognitive function and mood. https://www.youtube.com/embed/dLokEBiXgBg?wmode=transparent&start=0 Some foods can negatively affect your memory and mood.
Sugar, saturated fats and ultraprocessed foods

Excess levels of some nutrients can also have detrimental effects on the brain. In humans and animal models, elevated consumption of refined sugars and saturated fats – a combination commonly found in ultraprocessed foods – promotes eating by desensitizing the brain to the hormonal signals known to regulate satiety.
Interestingly, a diet high in these foods also desensitizes the taste system, making animals and humans perceive food as less sweet. These sensory alterations may affect food choice as well as the reward we get from food. For example, research shows that people’s responses to ice cream in brain areas important for taste and reward are dulled when they eat it every day for two weeks. Some researchers think this decrease in food reward signals may enhance cravings for even more fatty and sugary foods, similar to the way smokers crave cigarettes.
High-fat and processed-food diets are also associated with lower cognitive function and memory in humans and animal models as well as a higher incidence of neurodegenerative diseases. However, researchers still don’t know if these effects are due to these foods or to the weight gain and insulin resistance that develop with long-term consumption of these diets.
Time scales
This brings us to a critical aspect of the effect of diet on the brain: time. Some foods can influence brain function and behavior acutely – such as over hours or days – while others take weeks, months or even years to have an effect. For instance, eating a slice of cake rapidly shifts the fat-burning, ketogenic metabolism of an individual with drug-resistant epilepsy into a carbohydrate-burning metabolism, increasing the risk of seizures. In contrast, it takes weeks of sugar consumption for taste and the brain’s reward pathways to change, and months of vitamin C deficiency to develop scurvy. Finally, when it comes to diseases like Alzheimer’s and Parkinson’s, risk is influenced by years of dietary exposures in combination with other genetic or lifestyle factors such as smoking.
In the end, the relationship between food and the brain is a bit like the delicate Goldilocks: We need not too little, not too much but just enough of each nutrient.
This article was written by Monica Dus for The Conversation under a Creative Commons license. Read the original article.